“You have cervical cancer.”
A cervical cancer diagnosis can be terrifying, and it can take you by surprise.
It’s perfectly normal (and understandable) to feel completely overwhelmed. You may have questions about everything, from how you got it to whether or not you will be able to have kids.
Are you one of the 12,820 women in the U.S. diagnosed with cervical cancer each year? Here are the answers to some of your most important questions.
What exactly is cervical cancer?
It’s a cancer of the cervix—the lower part of the uterus (womb).
In nearly all cases, cervical cancer begins with a human papillomavirus (HPV) infection—the sexually transmitted infection that almost every sexually active person gets at some point in their lives.
Usually, HPV clears up on its own within 2 years, causing no symptoms or long-term health problems. But for others, the HPV can linger. If it does stick around, it can cause changes to the cells in your cervix. And in some cases, those changes can lead to cervical cancer.
Enough about how you got it. Let’s move onto what you really want to know—how it’s going to affect your life now.
It’s the burning question: Will I be okay?
Of course, it’s scary to find out you have a cervical cancer diagnosis. But you can sit back and take a few deep breaths.
When found early, cervical cancer is one of the easiest cancers to treat. Nearly half of women with cervical cancer catch it in its earliest stage. At that stage, the 5-year survival rate—percent of women who live at least 5 years after the cancer is found—is 91%.
What are the treatment options for cervical cancer?
There are several different types of treatment. Your physician will work with you to decide the best plan based on the cancer’s stage, your medical history, and your preferences.
The most common treatments include:
- Surgery to remove tumors or abnormal cells
- Radiation therapy to kill cancerous cells (via high-energy X-rays or radioactive particles)
- Chemotherapy to kill cancerous cells (via anti-cancer drugs injected into your bloodstream)
- Targeted therapy to stop changes in cancerous cells (via drugs targeted towards specific changes)
What about complementary or alternative medicine?
It’s a little bit difficult to get into whether or not complementary or alternative treatments—ones not within the scope of standard medical practice—are effective.
There isn’t much reliable information about these treatments, and some can even be harmful (e.g., certain herbs can cause liver damage, some vitamins can lower the effectiveness of chemotherapy, etc.).
If you’re looking to go the complementary or alternative route, look into integrative medicine. This is a combination of standard treatments (surgery, radiation), with some complementary and alternative approaches.
Integrative medicine has been shown to be safe and effective at treating mind, body, and soul.
No matter what, if you’re considering using any type of complementary or alternative medicine, talk to your physician first.
Can I still get pregnant?
It depends. If your cancer has gone away, and treatments haven’t damaged your reproductive organs, you may be able to get pregnant.
Some treatments, like radiation or chemotherapy, can cause infertility, but not always permanently. You might go back to menstruating and being able to conceive.
Other treatments guarantee that you won’t be able to get pregnant. Some women with cervical cancer are treated with a hysterectomy—surgery where your entire uterus is removed. Since the uterus is where a baby grows, you can’t get pregnant without it.
I was just diagnosed—and I’m already pregnant. Will my baby and I be okay?
The good news: Cancer rarely affects a fetus directly.
Not quite as good news: Cancer can make things a bit more complicated for the mother and physicians.
The biggest effect of pregnancy on cancer is when and how your cancer gets treated. When choosing the time to start treatment, there are several factors your treatment team will consider, including:
- How far along you are when diagnosed: Some treatments are more likely to harm the baby during the first 3 months, so your treatment may be delayed until the second or third trimester.
- The stage of your cancer: If the cancer is caught very early on, your physician may want to hold off on any treatment until after delivery.
If your physician does want you to begin treatment during pregnancy, there are generally two safe treatment options:
- Surgery to remove the tumor: There is very little risk to the developing baby, so it’s considered the safest treatment option during pregnancy.
- Chemotherapy to destroy cancer cells: This option is not safe during the first 3 months of pregnancy, when the baby’s organs are developing. But during the second and third trimesters, chemotherapy is not considered risky.
Can I breastfeed during treatment?
It’s not recommended if you’re using chemotherapy or radioactive drugs. These can be passed on to your little one through your breast milk, harming your baby.
How is cervical cancer different in Black women?
Cervical cancer can affect any woman, regardless of skin color. However, it does affect Black women a little differently.
There is a noticeable difference between the amount of Black and white women diagnosed with cervical cancer. The cervical cancer incidence—the rate of newly diagnosed cases of a disease—is 41% higher in Black women.
Mortality rates are also different.
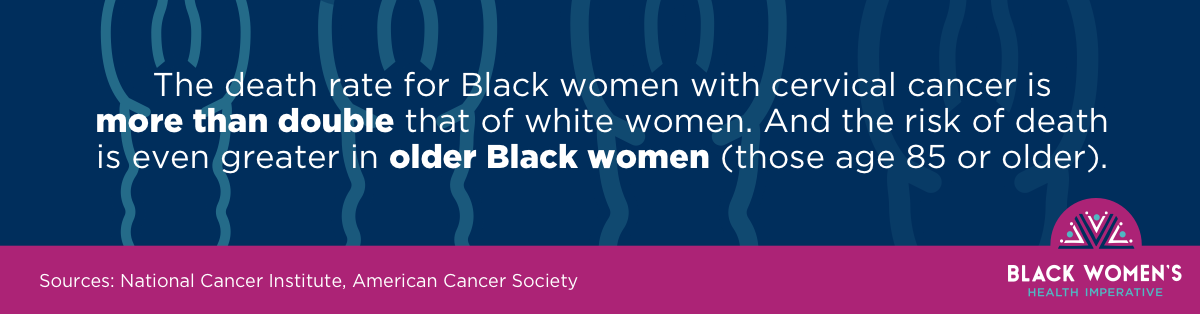
Why is that?
There are many reasons why both diagnosis and death rates are higher in Black women than in white women:
- Black women are less likely to get—or even know about—the HPV vaccine (the medication which prevents some of the types of HPV that can cause cancer).
- Even if they do get the vaccine, they might not have as good a level of protection as white women. The vaccine only protects against a few of the HPV types that can cause cancer, and Black women tend to have the types that the vaccine does not protect against.
- Outside factors, like stigma, fear, and cultural beliefs, can cause Black women to hold off on getting screened or receiving follow-up care. That means that by the time the cancer is caught or treated, it may already be past the early stages, making treatment less successful.
- Compared to white women, Black women often have less access to health care, or receive lower-quality care.
Once I’ve beaten this, how can I stay healthy?
First, you should celebrate, You’ve been through one heck of an ordeal, and you deserve to treat yourself. But once the post-cancer festivities have slowed down, it’s time to make a game plan.
One of the most important things to do is keep up your overall health so you don’t run the risk of getting a second cancer. Stay at a healthy weight, keep up physical activity, eat a healthy diet, and keep alcohol use at a minimum.
If you’re a smoker, put down the cigarettes. Smoking is known to increase the risk of several of the second cancers that are more common after cervical cancer.
It’s also important to take care of your whole self. Cancer can take a huge toll on your mental and emotional health, and that toll doesn’t automatically disappear once you’ve beaten cancer.
Look for survivor support groups (either in person or online), talk to a therapist, meditate, paint, play an instrument—anything that helps restore your spirit and soul.
Talk to your physician about follow-up care (e.g., check-up appointments, screenings for second cancers)—and stick to it.
Do you know someone else going through cervical cancer? Make sure she has the facts, too.